Sleep apnea, a condition marked by interrupted breathing during sleep, has long been studied predominantly in men, leading to a significant disparity in understanding its effects on women. As research delves deeper into this disparity, it's becoming increasingly evident that women experience sleep apnea differently, from symptoms, to risk factors, necessitating a shift in awareness and diagnosis protocols.
While it's estimated that over 20 million Americans live with sleep apnea, recent studies suggest that this number might be significantly higher due to underreporting and misdiagnosis, particularly among women. Women often present with symptoms that diverge from the stereotypical signs associated with sleep apnea in men.
Within medicine as a whole, there is a gender bias. A lot of the studies are done with men versus women. One of the main reasons women weren’t included in sleep studies is because women are so complex. Meaning there may be emotional or hormonal reasons that can lead to insomnia.
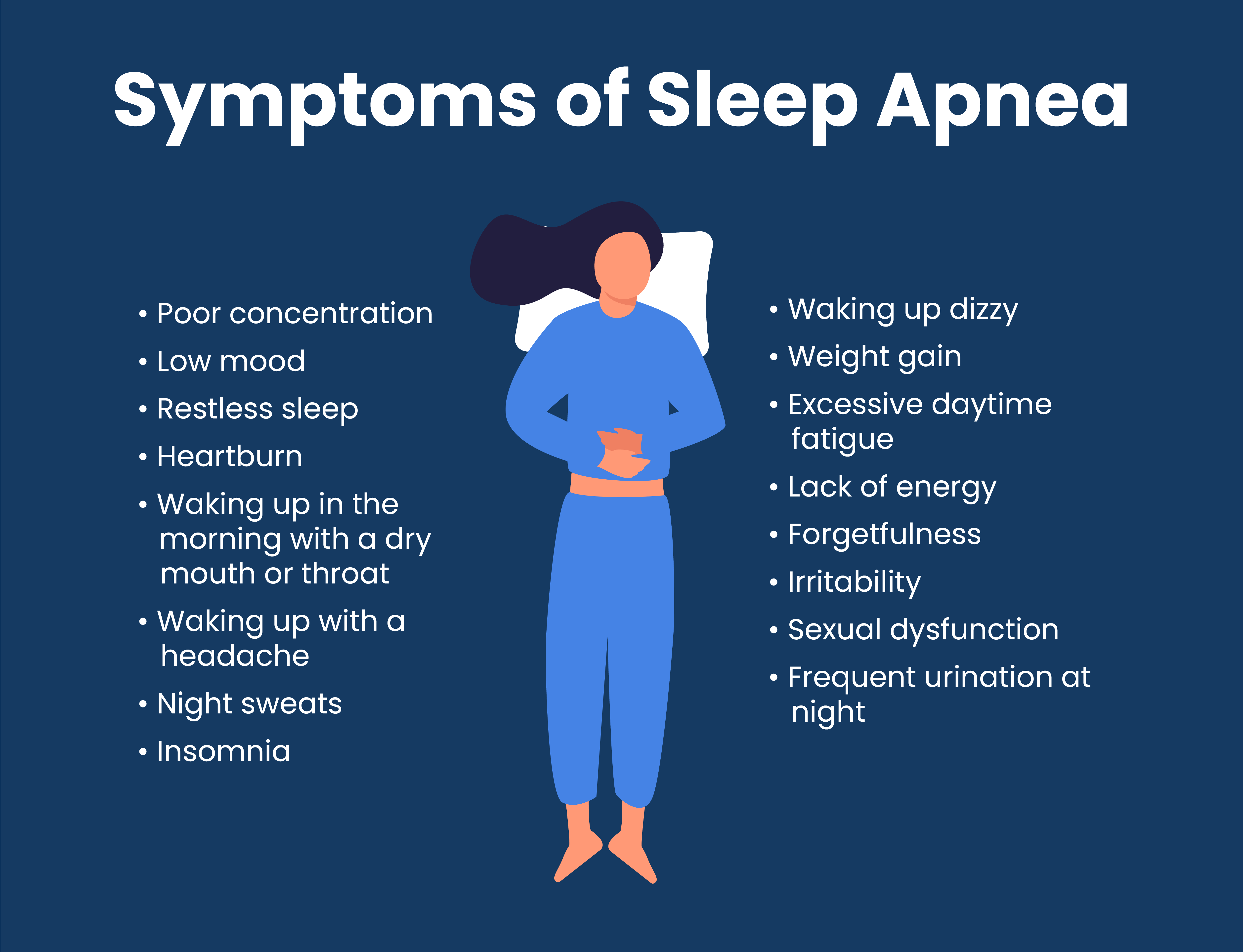
Unlike men, who commonly report symptoms like excessive snoring and obesity, women may exhibit subtler signs such as anxiety, insomnia, depression, restless legs, morning headaches, and daytime sleepiness. Snoring, though less prevalent, remains a notable symptom among women with sleep apnea.
Women’s brains are more active at night, meaning when their airway starts to partially collapse, their brains will wake them up before they completely collapse. Women can have more subtle symptoms from Obstructive Sleep Apnea.
Women face distinct risk factors for sleep apnea, including hormonal changes during pregnancy and menopause. Pregnancy-related hormonal shifts and changes in upper airway structure increase the likelihood of developing sleep apnea, leading to potential complications such as gestational diabetes and hypertension. Similarly, the drop in estrogen levels during menopause heightens the risk of sleep apnea, particularly in postmenopausal women. Additionally, conditions like polycystic ovarian syndrome (PCOS), characterized by hormonal imbalances and increased testosterone levels, elevate the susceptibility to sleep apnea among women.
Feeling tired, and sometimes it’s normal because it’s so common. But it doesn’t mean there couldn’t be an underlying condition like Obstructive Sleep Apnea because rates double to triple from pre-menopause and post-menopause.
Given the propensity for misdiagnosis, women experiencing symptoms of sleep apnea should advocate for themselves and discuss their concerns with healthcare providers. It's crucial to emphasize the need for a thorough evaluation, including a sleep study, to diagnose and treat sleep apnea accurately. Symptoms such as depression, menopausal changes, and insomnia, while valid concerns, may not address the underlying sleep apnea and warrant specialized attention.
As awareness grows and research continues to uncover the nuances of sleep apnea in women, it's imperative to bridge the gender gap in understanding and addressing this condition. By recognizing women's distinct symptoms and risk factors, healthcare professionals can provide tailored care and support, ultimately improving outcomes and quality of life for all individuals affected by sleep apnea. If you suspect you may have sleep apnea, don't hesitate to initiate a conversation with your healthcare provider and advocate for the comprehensive evaluation you deserve.
Find a doctor who can help with screening, diagnosis and treatment of snoring and/or sleep apnea CLICK HERE or email info@app-nea.com